*Editors Note: Informeret will be taking a Christmas break. Our last edition of the year will be the Monday Morning Report on Dec 19. We will be back in the New Year.*
🦠Pandemic🦠
🇩🇰
COVID numbers continue to climb in Denmark. Pandemic indicators almost across the board kept rising last week, according to the latest weekly assessment from the Statens Serum Institute.
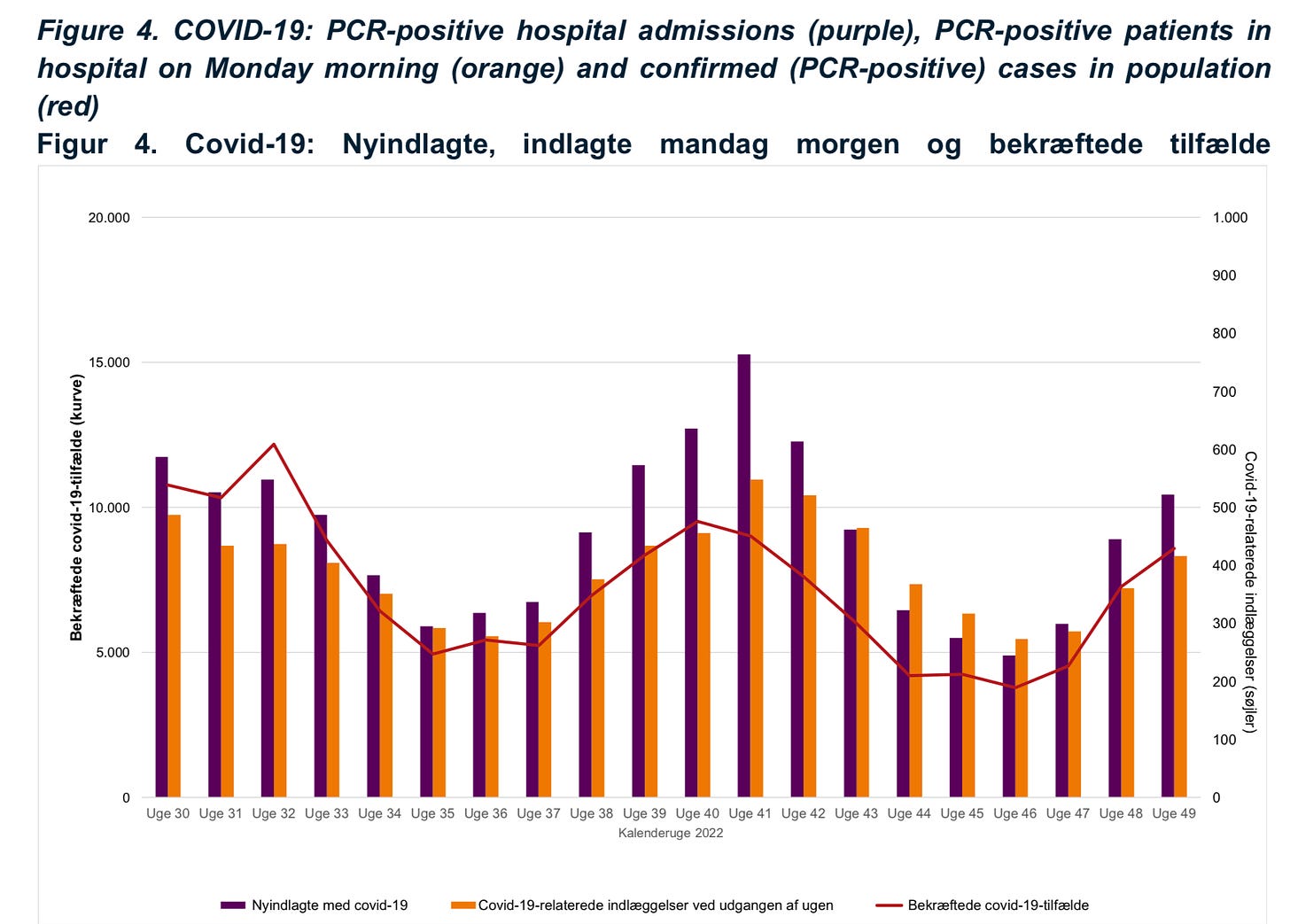
The COVID incidence rate rose from 123 cases to 145 cases per 100,000 people. The positivity percentage also crept upward, going from 18% to 19%. The number of PCR tests administered also increased by 11% week to week.
Among vulnerable seniors in care, infection numbers increased for a fourth straight week. There were 35 hospitalizations among nursing home residents, seven more than the week before. After four weeks of a stable number of pandemic fatalities among senior home residents, there were 11 deaths last week, a slight increase from the eight lives lost the week prior. Infection activity is also rising among senior home staff and hospital employees.
Infection activity rose again across all five Danish regions. Region Sjælland had the highest incidence rate with 173 per 100,000 people. While, Region Midtjylland recorded the highest positivity percentage with 24%.
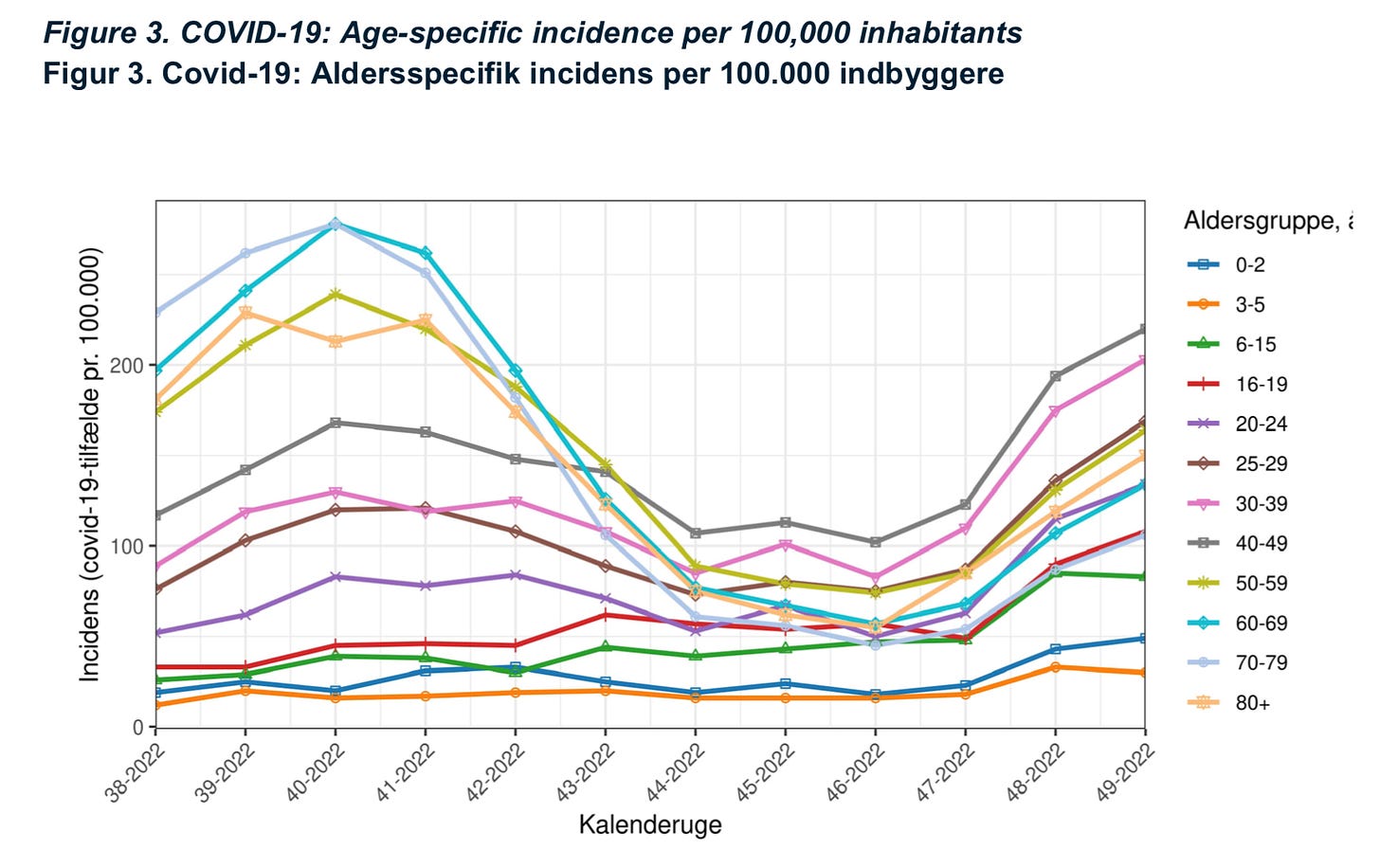
Looking at the pandemic situation by age, coronavirus activity increased in every age group except for those three to 15 years old where numbers fell. For a sixth week in a row, those 40 to 49 years old saw the highest COVID incidence rate (220 per 100,000 people).
The positivity percentage also rose across almost every age group, save kids three to 19 years old, where the rate declined a little. Those six to 49 years old had the highest positivity percentage (26%).
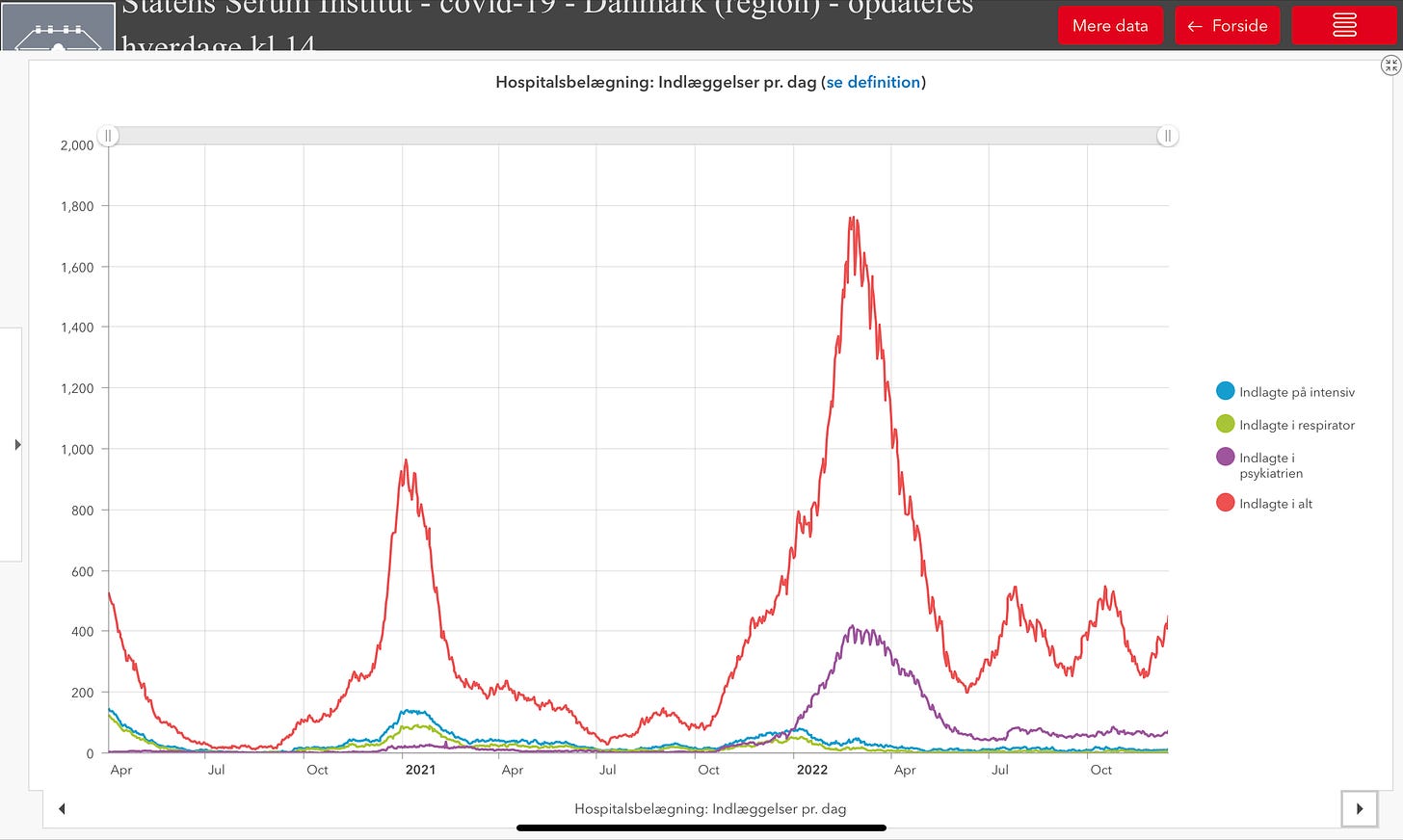
COVID hospitalizations are climbing, with 522 pandemic-related admissions last week; that is 77 more than the week before. As has been the case all year, seniors 70 to 89 years old continue to make up the largest proportion of new infection-related admissions.
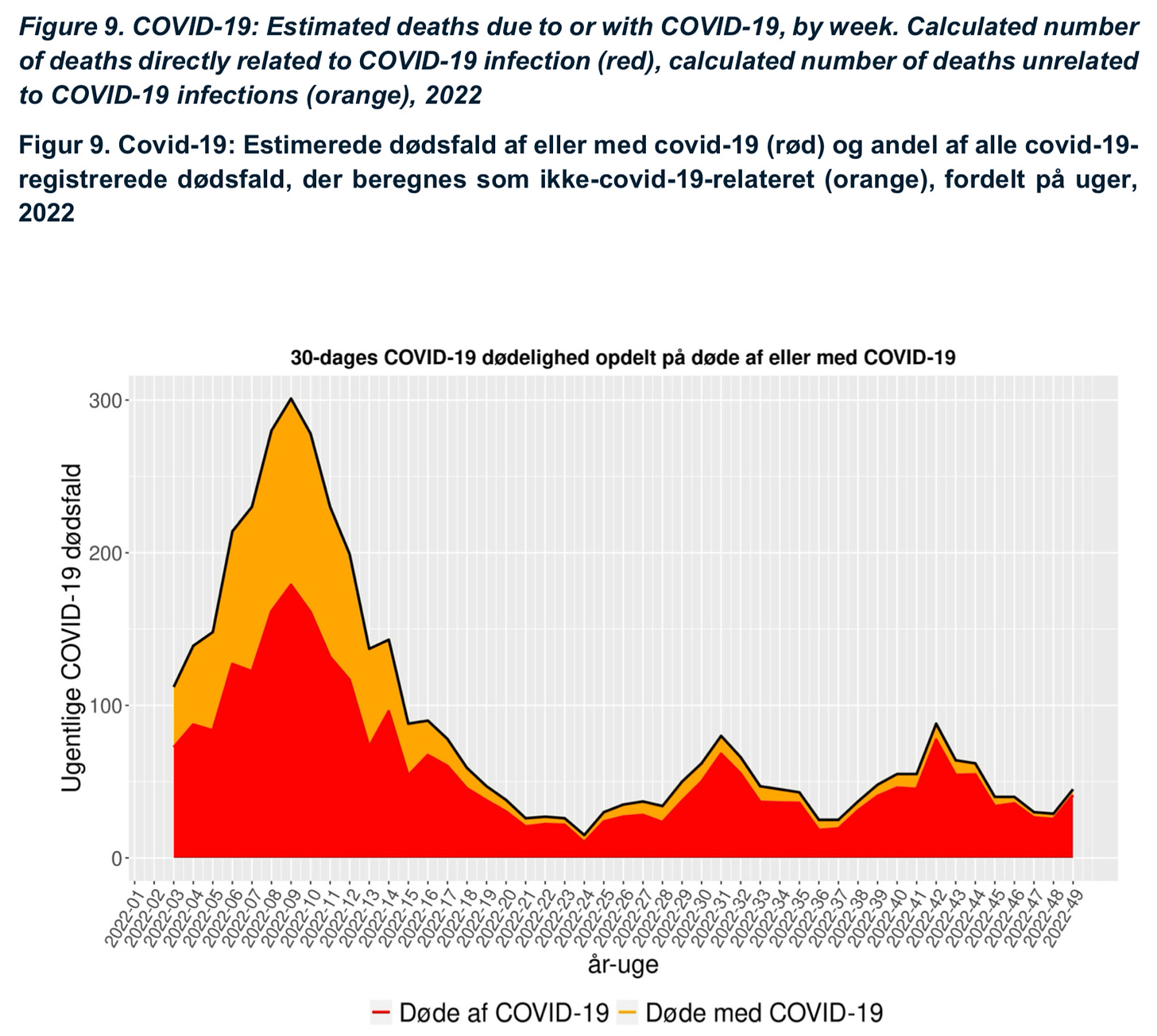
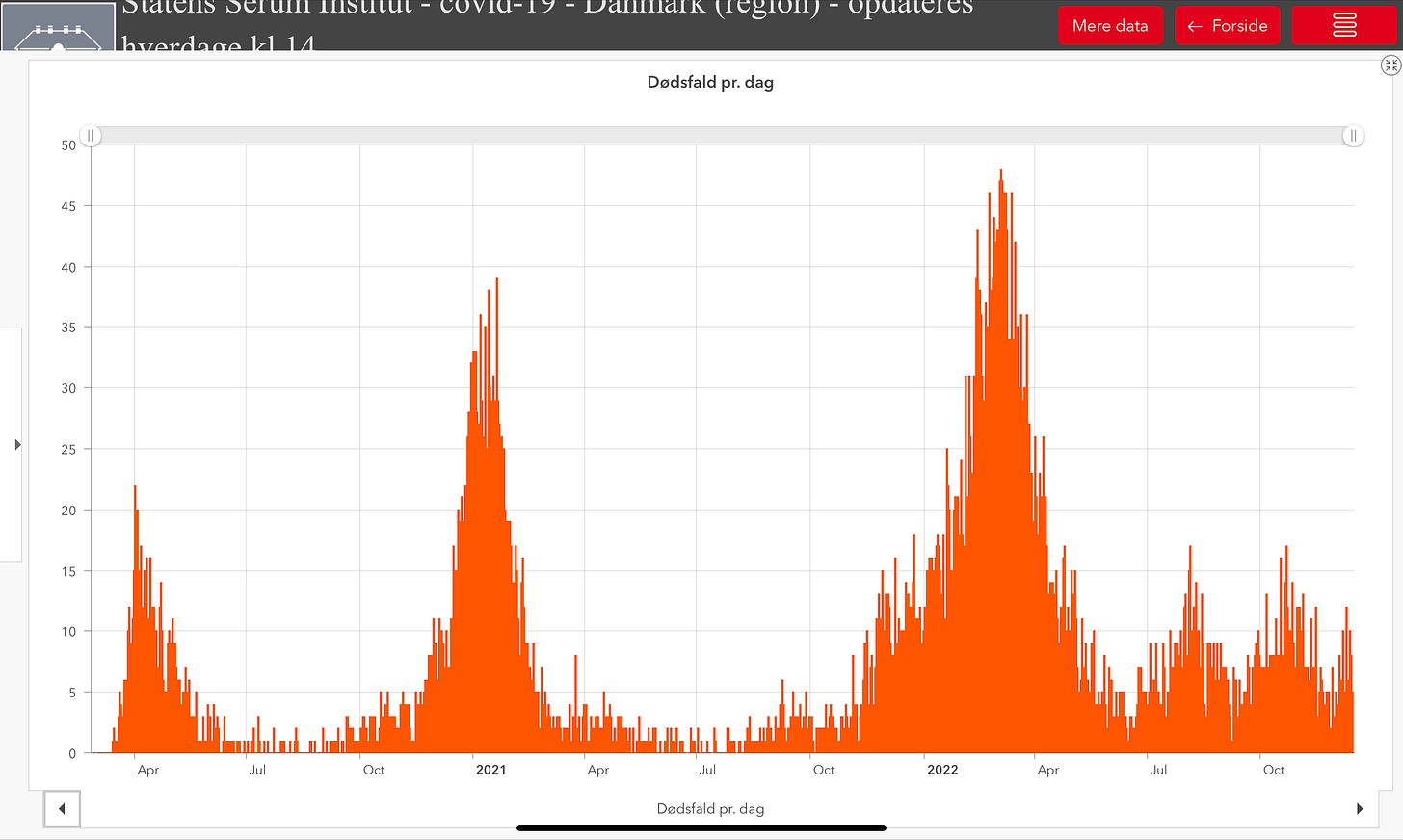
Pandemic deaths jumped last week with 45 more lives lost to coronavirus, that is 16 more than the previous week.
On the variant front, BA.5 and its sub-variants continued to remain dominant in Denmark last week, but just barely. The concerning BQ.1.1 variant and its sub-variants made up 37% of all sequenced positive test results last week. BA.2.75 also continues to increase its share of infections, now accounting for 20% of all cases. While the recombinant XBB strain also continues to grow and was responsible for 7% of all infections in week 49. The new variants all have one thing in common, a greater immune escape allowing them to slip around antibody protection to reinfect people.
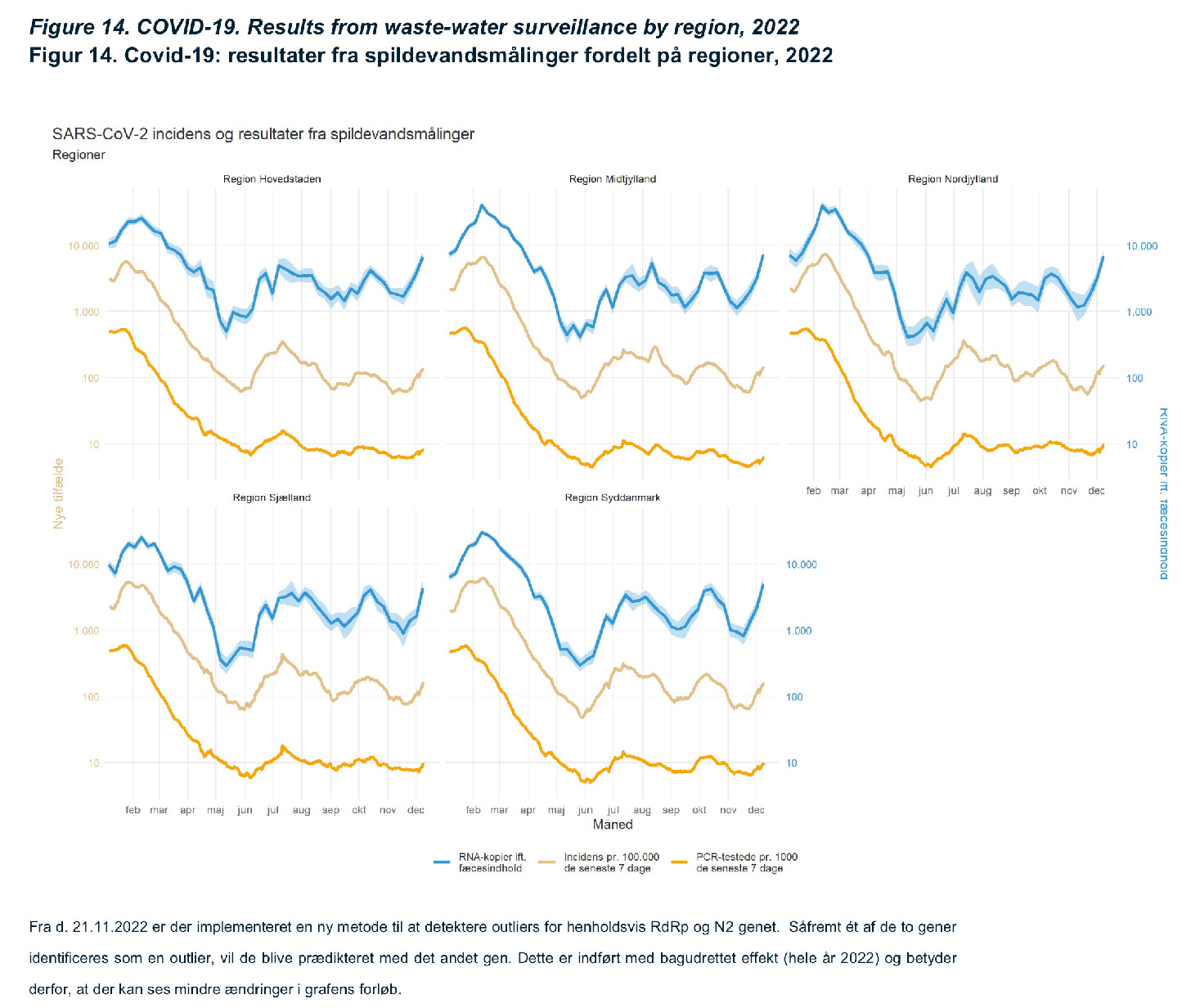
COVID wastewater surveillance shows coronavirus activity is increasing nationally across Denmark and across all five Danish regions. The SSI is reporting a “very sharp increase” in the weekly growth rate over the last three weeks. On the wastewater side, it is the BQ.1 variant that is the most dominant, accounting for 41% of all sequenced testing.
-
COVID hospitalizations (452) have jumped day over day (+43) while the number of severely infected people in an ICU (13) also crept up (+2) of those, the number on a ventilator (4) is unchanged.
Infection admissions into a psychiatric facility (74) also rose (+8).
-
Denmark has reported 1,341 COVID infection (underreported), including 634 reinfections, and 6 more coronavirus deaths in the last day.
With 7,228 PCR tests yesterday, the positivity percentage equals 18.55%, which is an increase. Over the last seven days the rate is 19.4%.
-
On the vaccination front, 32% of the total population now has a 2nd COVID vaccine booster dose. 75% of the target group, those 50 years old and older, have another vaccine booster shot, and 88.4% of all vulnerable seniors in care also have a 4th dose.
-
The Statens Serum Institute is emphasizing the effectiveness of COVID vaccines by pointing to hospitalization numbers. It notes that among those 50 years old and older who had another booster dose, the hospitalization rate was 13 per 100,000 people. The rate is double for those in the same age group who are unvaccinated or who haven’t yet had a 4th dose.
-
Denmark finally has a new government, six weeks after the national elections. This marks the longest ever negotiating period in Denmark between an election result and the official forming of a new government.
Of note for topics we cover in this newsletter, Denmark has a new Climate, Energy, and Supply Minister and he comes from outside the parliament. The former Director of Dansk Energi, Lars Aagaard, has been tapped for the job.
Aagaard has been dubbed Denmark’s “Mr. Energy” and he told DR that he is “insanely proud and humbled” to have been chosen for this new role.
Another Danish minister who has been mentioned a lot in this newsletter is now former Health Minister Magnus Heunicke, who is the new Minister of Environment. Venstre’s Sophie Løhde takes his old job in the newly named Minister of the Interior and Health.
-
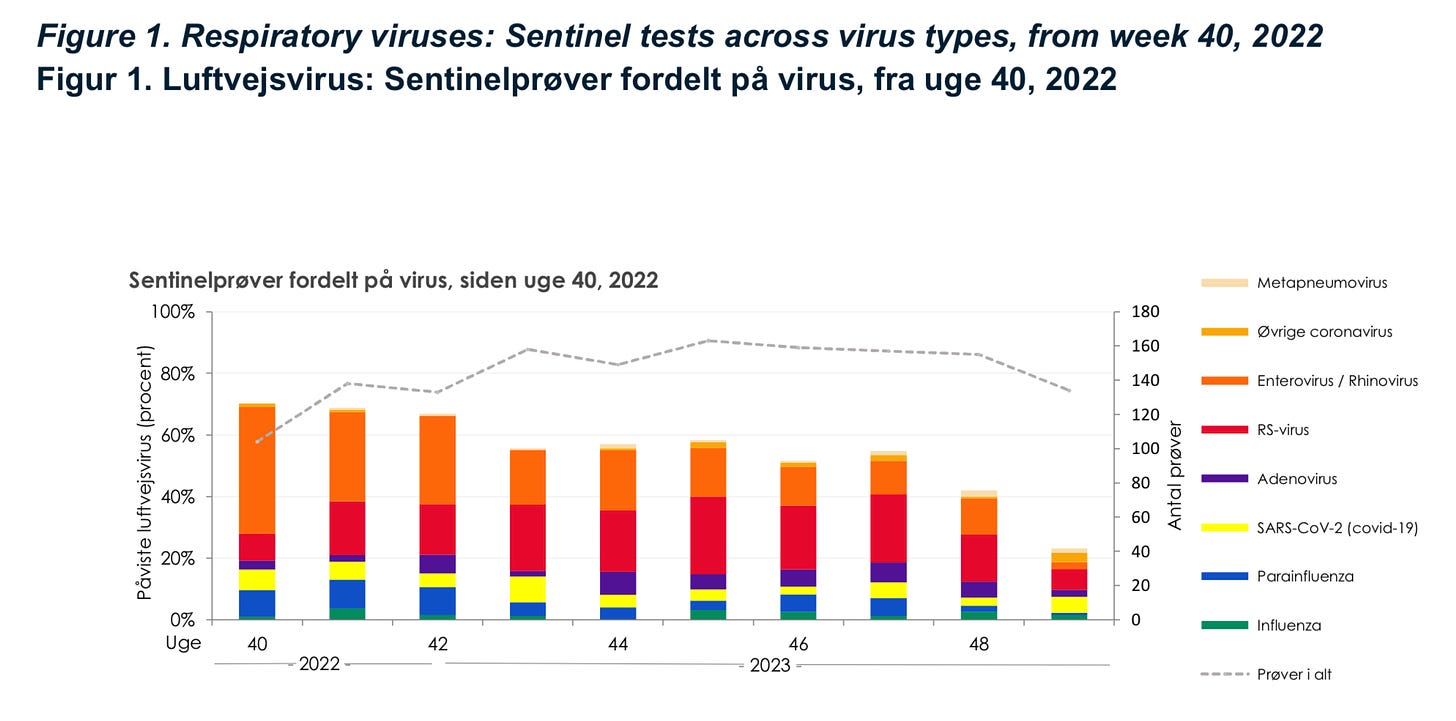
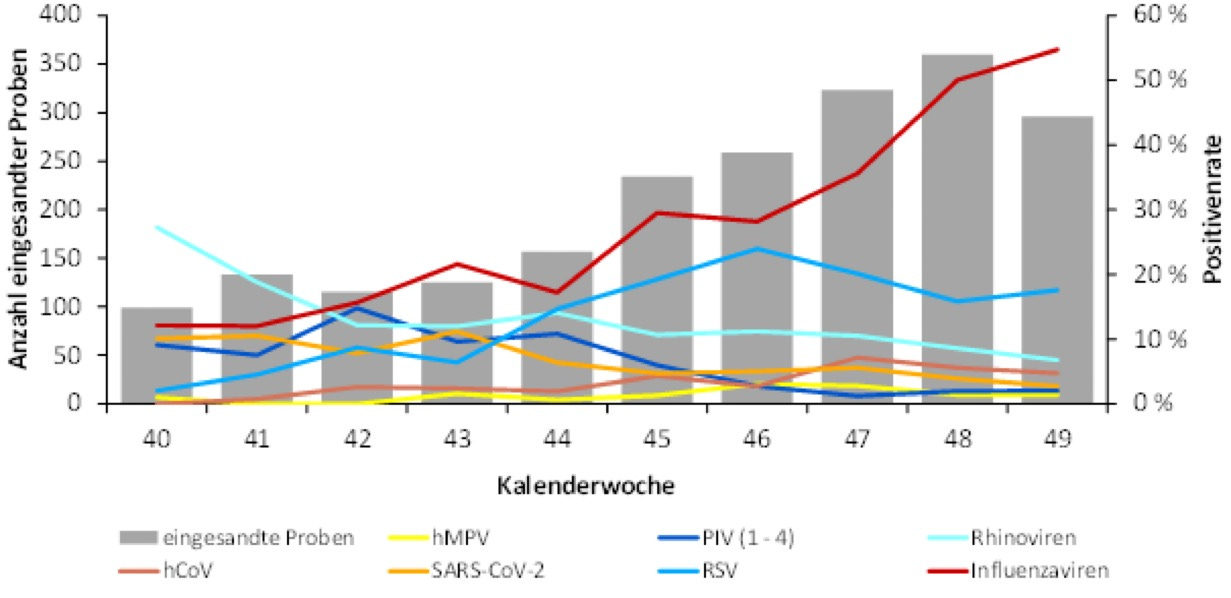
The Statens Serum Institute’s sentinel surveillance system found that besides coronavirus, it was the RS virus, enterovirus, and rhinovirus that made up the most respiratory infection activity in week 48, two weeks ago.
But, the SSI notes that while RS virus cases decline, but still remain higher than virtually every other year prior to the pandemic, influenza activity has “increased sharply” albeit still within ‘normal’ levels for this time of year.
🇸🇪
Sweden has added 11,333 (wildly underreported) new infections and another 130 corona deaths; both numbers are big increases week to week.
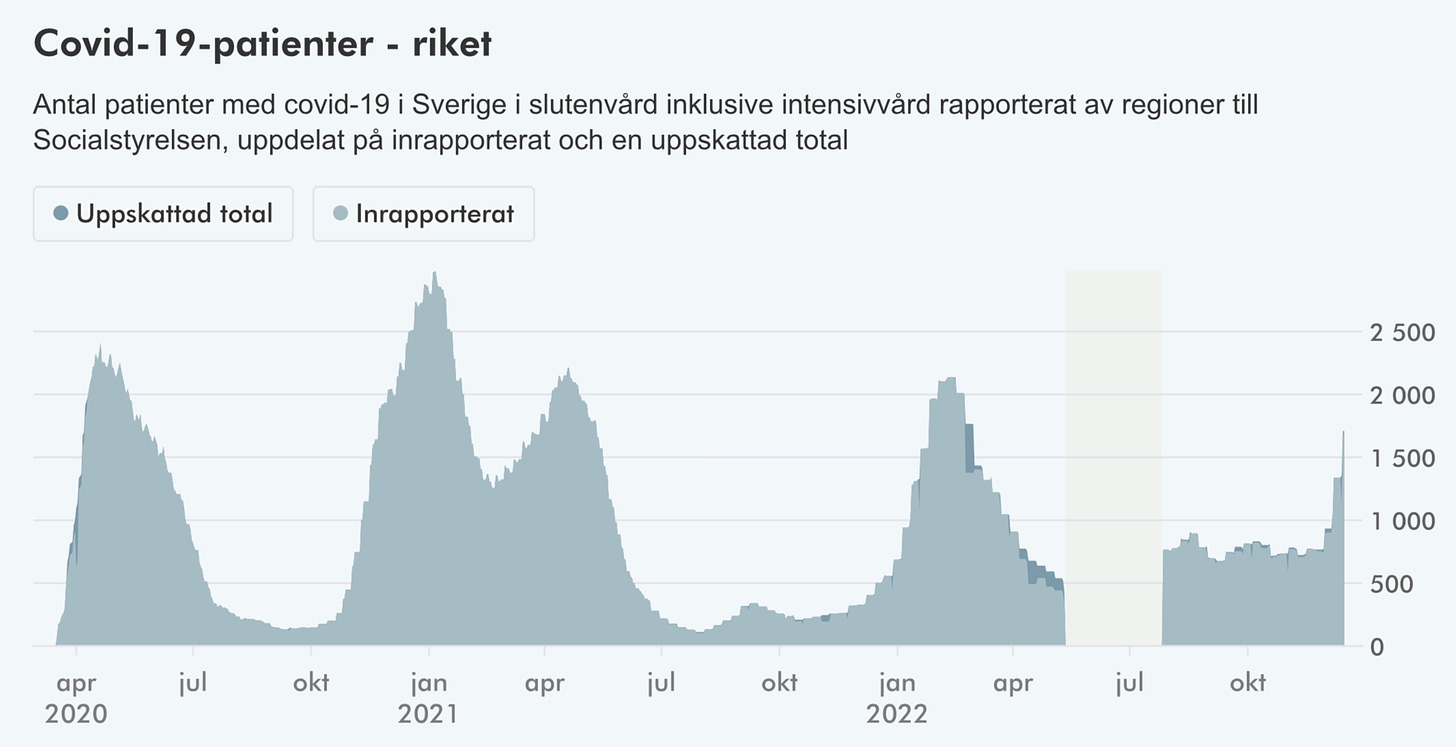
COVID hospitalizations (1,678) continue to soar (+339) while ICU numbers (23) dropped (-5).
Of those eligible, 81.1% of seniors 65 years old and older have a 2nd booster dose.
-
As Sweden’s COVID numbers rocket upwards, it doesn’t sound like the situation is going to improve anytime soon. The Swedish Public Health Agency warned on Thursday that coronavirus, RS virus, and influenza infections will all continue to “sharply increase.” The agency says getting vaccinated for COVID and influenza is the best way to reduce the chances of severe infections, hospitalization, and death, especially for vulnerable at risk groups and seniors. It adds that it is also important to stay home when you are sick.
As coronavirus infections spread the health authority says it is seeing an increase in interest in getting vaccinated.
State Epidemiologist Anders Lindblom:
“We see that interest in updating vaccine protection against COVID has increased. It is gratifying and very important now that the spread of infection is increasing. Above all, many people have taken a booster dose, but there are still many people left who need to take their 4th dose.”
Sweden currently offers a 2nd COVID vaccine booster for high-risk populations between the ages of 18 to 64 and vulnerable seniors 65 years old and older. For everyone else, it deems three doses to be sufficient.
Infants are at highest risk of severe RS virus and influenza infections. The health agency advises parents to take every precaution to protect their youngest children. This includes frequent hand-washing, washing commonly touched surfaces, and keeping them away from anyone who is sick or symptomatic.
The agency says in the weeks ahead, coronavirus, RS virus, and influenza infection activity “will continue to increase.” It warns that hospitals, already under strain, are going to face even more pressure as cases rise; so will severe infections requiring hospital care. This will be exacerbated by healthcare workers also getting sick.
-
Add another one to the list. The Swedish Public Health Agency is warning that cases of winter vomiting disease are spreading with infections “gaining momentum.”
Epidemiologist Elsie Ydring:
“How extensive the infection spread will be this season we cannot yet say. Last year, the season was tougher than usual with many reported cases. Also, for the first time ever we saw two peaks in one season, usually we only see one peak which usually falls in February or March. The more severe season was probably an effect of the fact that hardly any cases were reported the year before [due to the pandemic].”
The bacteria causing winter vomiting disease is quite contagious and the health agency that regular hand disinfectant doesn’t have much effect. It advises regular and thorough washing using water and soap.
🇫🇮
Finland registered 10,537 infections over the last seven days while losing another 211 lives to the pandemic.
COVID hospitalizations (904) dipped slightly (-7).
Currently, 20.8% of the total population has a 4th COVID vaccine dose.
-
Get vaccinated now. That is the message from the Finnish Institute for Health to anyone who hasn’t had a COVID vaccination or a 2nd booster dose. The advice also applies for getting your flu shot as health officials note the fast approaching holiday season.
Chief Physician Hanna Nohynek:
“Many vaccination venues are closed on holidays and the in-between days, so you should get the recommended vaccine doses for both coronavirus and influenza before Christmas, if possible. Many people meet their loved ones at Christmas, so it would also be good if protection was in place before then.”
The institute says there are well over a million people in Finland who have yet to get a 2nd COVID booster dose. There are around two-million people eligible for a booster dose in Finland, with about 600,000 booster doses administered so far.
“If you belong to a risk group, you should still take the booster dose. It must also be remembered that there are significantly fewer coronavirus infections in the elderly than in the younger population. Many therefore lack appropriate protection against severe COVID infections.”
The institute says it also has lots of influenza vaccine doses left, including 116,000 doses of the special nasal pediatric doses.
“The influenza epidemic has started. The number of influenza cases reported to the Infectious Disease Registry has increased in recent weeks. Both influenza A virus types and influenza B viruses have been found in Finland.”
The agency warns that with both coronavirus and influenza circulating, it is possible to be infected with both at the same time.
“It's worth taking both vaccines, because getting sick with corona and influenza at the same time can be a serious situation.”
🇳🇴
Norway’s latest COVID wave is still increasing but at a slower rate, according to the latest weekly pandemic snapshot from the Norwegian Institute for Public Health. The update doesn’t paint a pretty picture as hospitals strain under not one but three epidemics.
For a 9th straight week the number of COVID infections, an unreliable statistic due to a lack of testing, has continued to increase.
After 10 weeks of rising COVID hospitalizations, the institute says admissions leveled off last week, with 289 new pandemic patients, just six more than the week previous.
Another 57 lives were lost to the coronavirus in Norway last week. For the last six weeks, the weekly death toll has bounced between 43 and 65 deaths.
COVID wastewater surveillance, which had shown increasing virus activity for eight straight weeks, saw a slight decrease in COVID activity last week. Wastewater surveillance in Norway is a little limited as it only covers about 30% of the population.
The number of coronavirus outbreaks in Norwegian hospitals is growing, with 26 reported last week, up from the 22 of the week previous..
As of the end of last week, 72% of seniors 75 years old and older had a 2nd booster dose. Among those 65 to 74 years old, the vaccination rate is 64%.
The agency says RS virus infections are also rising rapidly “with more and more” hospital admissions, especially among young children. RS virus-related hospital admissions also continued to shoot upward, with 144 last week, a significant increase from the week before, where there was 73.
With the influenza positivity percentage increasing to 11% last week, a four-point rise, the NIPH says it is expecting a “significant contagion” over the Christmas holidays.
The BQ.1.1 variant is now dominant in Norway.
The NIPH says influenza infections are “increasing rapidly” as are flu-related hospital admissions, with the epidemic in full swing. There were 163 flu-related hospitalizations last week, a big increase from the 95 of the week prior. The Institute says a “very low proportion” of children (6.4%) have had their flu shot and coverage is also much too low across all the eligible groups, especially among healthcare workers (35%) and those in high-risk and vulnerable populations, which is concerning considering the looming Christmas season.
-
Norwegian health authorities are urging people to be cautious and keep themselves safe over the holiday season. The Norwegian Institute of Public Health says it is important to follow infection control recommendations, especially with so many viruses circulating.
Infection Control Director Trygve Ottersen:
“The good news is that we don't need our own Christmas restrictions this year. But it is important to follow the few basic infection control recommendations we have for this winter season. Winter is the time for flu and other respiratory viruses, and we see that many people have coronavirus and that the flu is already on the rise.”
The recommendations in Norway are simply that people get their flu shots and COVID vaccinations, that they stay home if they are sick, wash hands frequently, and cough into their elbows.
-
Norway is seeing more cases of scarlet fever and strep throat than prior to the COVID pandemic. Both are quite common every year, especially among young children but after COVID restrictions saw streptococcal infections all but vanish; and in Norway, as in across Europe, with pandemic restrictions all gone, the bacteria is back with a fury.
NIPH Dr. Yngvild E. Bentdal:
“Parents should see a Doctor or go to an emergency room if the child has symptoms of scarlet fever to assess whether there is a need for antibiotic treatment.”
The NIPH says it is seeing evidence of ongoing scarlet fever outbreaks in Norway and recorded a historically high number of visits to a Doctor for strep throat compared to any year prior to the pandemic.
Earlier this week, the European Centre for Disease Prevention and Control issued a warning about severe streptococcal group A infections across Europe. So far, this hasn’t been an issue in Norway.
“We see no definite increase in the number of cases of severe streptococcal group A infections in Norwegian children in 2022 compared to before the pandemic. Nor does it seem that the bacterium has become more serious than before. But, this can change, so we are keeping a close eye on the situation.”
In rare cases, severe streptococcal group A infections, or iGAS infections, can cause blood poisoning, meningitis, or necrotizing fasciitis, the so-called flesh eating disease. The reason for concern this year is that the risk of a severe streptococcal infection increases when the immune system is already struggling. With COVID, RS virus, influenza, and a host of the other common viruses all making the rounds, the immune system, especially for young children, is under strain.
The NIPH says these are some of the symptoms of an iGAS infection.
High fever over 39 degrees in combination with one of the other symptoms
Poor general condition, is lethargic or difficult to wake up
Neck stiffness
Lingering Rash
Drinks and urinates little
Very severe pain usually in the arms or legs without any swelling or discoloration.
It advises anyone, but especially children, who have one or more of these symptoms to get to a doctor immediately.
🇩🇪
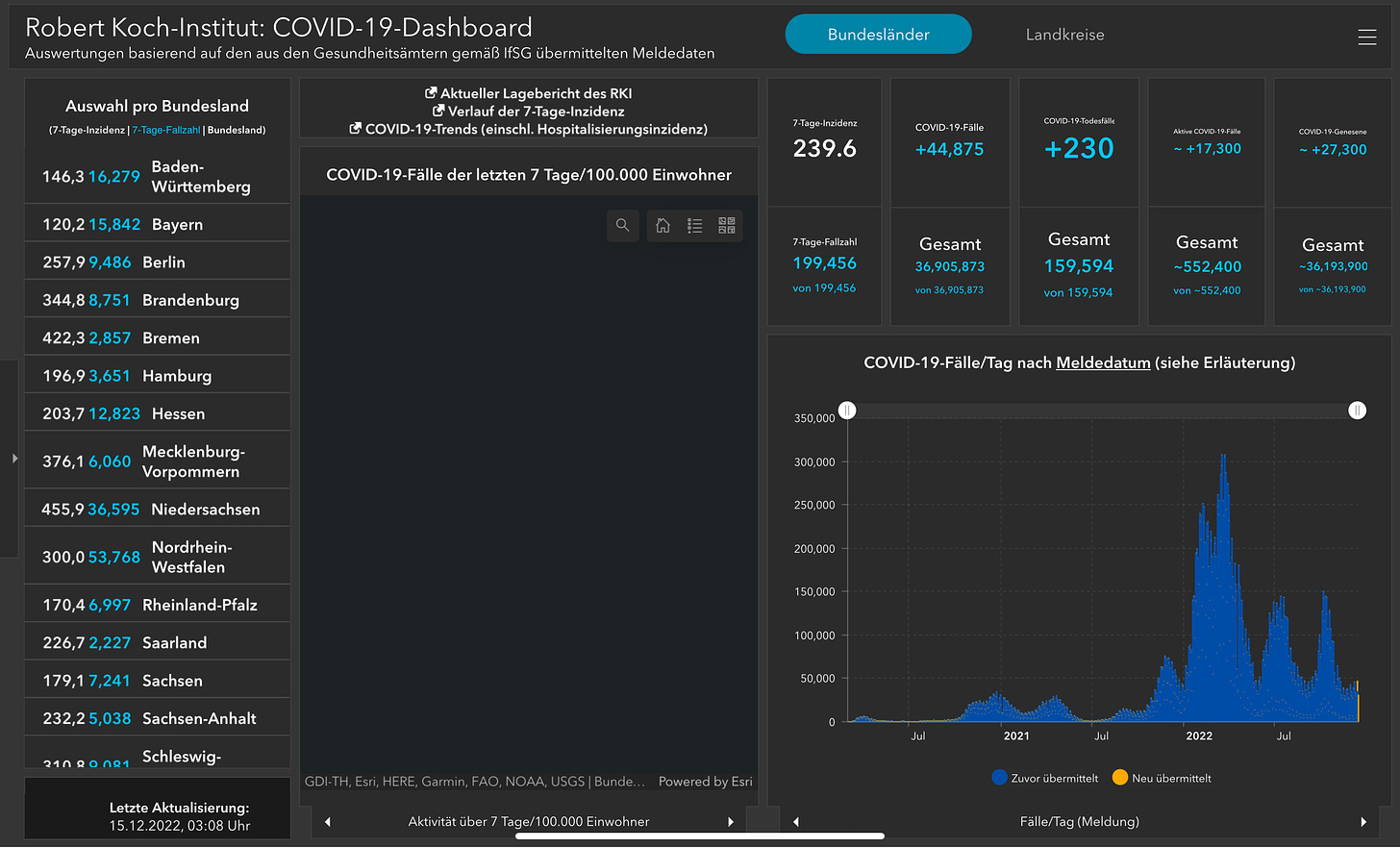
Germany recorded 44,875 new infections and suffered another 230 pandemic deaths in its Thursday update.
It added another 2,389 hospitalizations while ICU numbers (1,075) dipped slightly (-32). As a percentage of all intensive care beds in the country, pandemic patients are using 5.2%.
-
Germany is seeing a lot of influenza cases as the annual flu bug makes up 55% of the respiratory infections in the Robert Koch Institute’s sentinel surveillance program. RS virus trails behind at 18%.
The health agency says the infection pressure is high across all age groups as the seasonal effort kicks in with colder temperatures keeping us indoors where viruses have an easier time spreading.
The institute says it is seeing a lot of hospital admissions driven by the different respiratory infections, but especially influenza. Among infants, RS virus is the biggest cause for hospital admission at the moment.
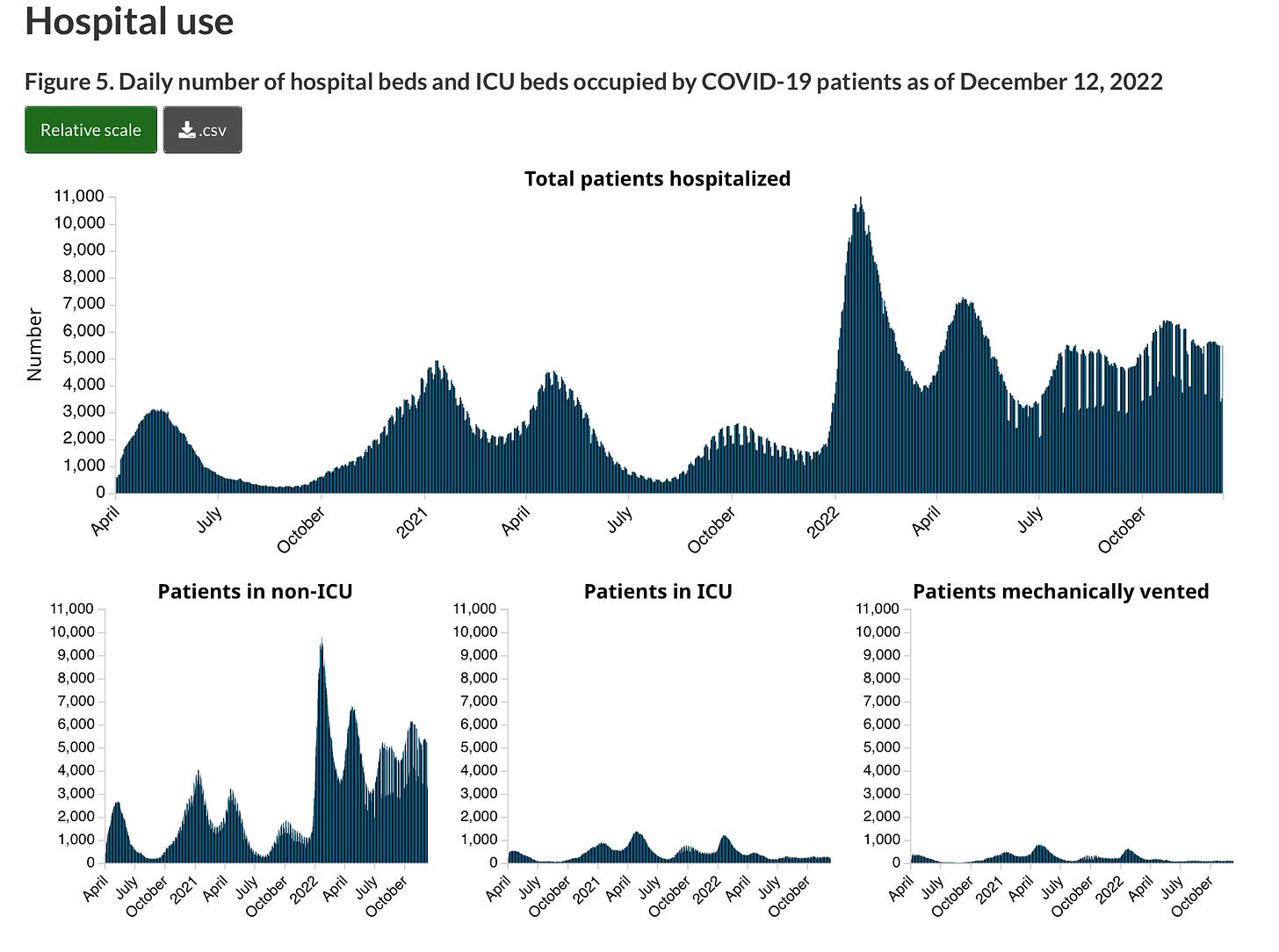
🇨🇦
A bit of a mixed bag on COVID hospitalizations across Canada. According to the latest numbers from the Public Health Agency of Canada, the total number of hospital beds being used by coronavirus-infected patients in the week ending December 12th was 5,488; that is 150 fewer beds in use than the week before. But, all the decreases were seen in General admissions, which fell by 159, to 5,288. Intensive care spaces headed in the opposite direction, increasing by nine to 260 severely infected people in an ICU. The number of people on a ventilator, 100, was also up, by eight.